The diagnosis of breast cancer with mammography
We have entered a technological age. Over the past 10 years, the diagnosis of breast cancer has
placed mammography at the forefront. No longer is a woman expected to find lumps and then
seek the care of a doctor. No longer is an annual or biannual examination by a physician expected
to detect breast cancer in its early stage, when it is most likely curable.
The majority of literature supports the contention that early diagnosis of breast cancer leads to
improved rates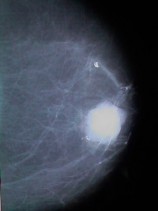 of survival. Literature also suggests that early diagnosis of breast cancer is best
accomplished with mammographic screening. Many clinically detected lesions are larger and
have a poorer prognosis than those lesions which are detected at an earlier stage on a
mammogram. Each year, more and more women are having annual mammographic screens.
of survival. Literature also suggests that early diagnosis of breast cancer is best
accomplished with mammographic screening. Many clinically detected lesions are larger and
have a poorer prognosis than those lesions which are detected at an earlier stage on a
mammogram. Each year, more and more women are having annual mammographic screens.
Mammography has assumed such an important role in breast cancer detection, that the
government has stepped in and begun to regulate the equipment and the practitioners involved in
these procedures. Mammography is often expensive, and the consumer expects value and has
great faith in technology and its practitioners. The science of medicine is superseding the art of
medicine.
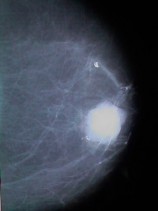
This mammogram shows a large cancer.
Failure to diagnose breast cancer has been and will continue to be a major allegation of medical
malpractice claims. In the past, the majority were unrelated to mammography. Now and in the
future, mammography will be epicenter of these lawsuits. Part of the reason is that more and more
women are having routine mammograms. By the time the cancer is detected on a mammogram, it
is likely that cancer has been present for a least one year. Some studies have suggested that up to
one third of prior mammograms show evidence of cancer, once the diagnosis is finally established.
Early diagnosis results in improved prognosis. The aggressive malpractice attorney will claim and
will inevitably find expert witnesses that will testify that the cancer can be seen on the earlier
mammogram. All the elements of a potentially successful lawsuit are present.
In reality, radiology is not practiced retrospectively. Subtle changes on a mammogram or any
other test can be and are overlooked by the most capable of doctors. Nevertheless, the argument of
medical experts in front of a jury, with the defense claiming that the mammogram was not
misread, are unlikely to exonerate the radiologist that misses a finding that another radiologist
states he can see. The public's expectations are high.
In addition to misinterpretation, there are other errors which occur and can lead to malpractice.
Many of these have to do with communication. Typically, radiologists have limited their
communications to referring physicians, who in turn communicate with the patient. The
inefficiency and the potential for errors in this chain of communication should be obvious.
Recently, federal legislation has required that mammography programs directly communicate the
results of the tests to the patient. This is a good requirement and will obviate some errors.
Failure in documentation can also result in malpractice. What if the wrong letter is sent? What if
the report is not received or has incorrect information? More and more radiology transcription is
being signed electronically, not eliminating the potential for patient misidentification. The
management of lesions which are probably benign occasionally results in the later diagnosis of a
malignant condition. Inappropriate reliance on biopsy results or other testing
in the face of a suspicious clinical exam can also have disastrous results.
Another result of aggressive mammographic screening is the pursuit of highly questionable
abnormalities which can result in unnecessary biopsies. The purist will maintain that it is
"better to
be safe than sorry." On the other hand, some biopsies can deform the breast. In addition, there are
other complications of surgery and of repeated biopsies. A proper balance between over diagnosis
and under diagnosis is badly needed. The threat of malpractice related to under diagnosis, will
tend to make physicians practice very aggressively. It remains to be seen whether lawsuits will be
filed when excessively aggressive search for breast cancer results in emotional or physical
scarring.
 of survival. Literature also suggests that early diagnosis of breast cancer is best
accomplished with mammographic screening. Many clinically detected lesions are larger and
have a poorer prognosis than those lesions which are detected at an earlier stage on a
mammogram. Each year, more and more women are having annual mammographic screens.
of survival. Literature also suggests that early diagnosis of breast cancer is best
accomplished with mammographic screening. Many clinically detected lesions are larger and
have a poorer prognosis than those lesions which are detected at an earlier stage on a
mammogram. Each year, more and more women are having annual mammographic screens.