
Sample patient profile
The patient is a 55 year old right-handed engineer who was an apparent good health until 1997. He started with frequent incapacitating headaches which were characterized by a progressive vice-like bilateral pain. This characteristically became worse without pharmacologic intervention, typically with Fiorinal. He attributed the headaches to stressful conditions at his workplace. In addition, anxiety, palpations, depression, and insomnia contributed to a feeling of ill health and reinforced the impression that the symptoms were psychological. In early 1998, the patient visited his family practitioner. Prozac and lorazepam were prescribed with some improvement.
The patient was referred to a neurologist for further evaluation of headaches. A MRI of the brain was normal. The neurologist diagnosed severe tension headaches and prescribed doxepin. In late 1998 additional symptoms of left shoulder pain and left arm weakness appeared. The pain was associated with tenderness medial to the scapula and was felt to be musculoskeletal in etiology. Trigger point injections were not helpful. Anti-inflammatory medication was not helpful. The only relief was with narcotic analgesic, particularly Vicoprophen.
After a few months of unrelenting and debilitating pain, MRI of the cervical and thoracic
spines was performed. There was a left paracentral disc herniation at C5 6.
Moderate scoliosis and degenerative change of the upper thoracic spine was present. Most impressive, however, was a vascular malformation
extending from T1 to T8, manifest by numerous intradural, extramedullary venous structures
posterior to the thoracic cord. Dilated paravertebral veins were also noted.
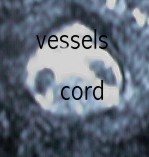
Axial MRI image to the left demonstrates two large vessels within the spinal canal, indicating a vascular malformation. Coronal MR image to the right shows curvature of the spine and dilated paravertebral vessels.
Neurosurgical consultation confirmed a vascular malformation of the upper thoracic region, with the help of additional MR angiography of the thoracic spine. Surgery was recommended, to be preceded by a vertebral angiogram. The patient has not yet consented to surgery, because of the high incidence of surgical complication.
Additional neurologic symptoms have occurred transiently, including left leg weakness and diplopia. The treating neurolgist believes these symptoms are due to vascular compromise related to the AVM.
The left shoulder pain has been replaced by right shoulder pain, especially with
abduction. A recent MRI of the left shoulder demonstrated a moderate joint effusion, severe
impingement, and severe tendonopathy without rotator cuff tear. Attempted joint aspiration was
unsuccessful, but was followed with a steroid injection into the joint. There was little improvement. A
rheumatologist was consulted, concluding that early neuropathic joint changes were most likely.
Neurontin was prescribed. The rheumatologist cautioned that surgical intervention for the
impingement might result in worsening.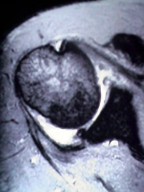
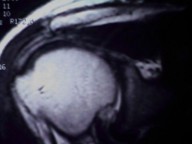
Axial MRI shows joint fluid [white] on the left, with labral degeneration. Coronal MRI image on the right shows edema of the supraspinatus tendon resulting from an impinging distal acromial spur.
Please note in schematic diagram to the right and below how the
supraspinatus portion of the rotator cuff is susceptible to
"impingement" as it courses inferior to the AC joint and the acromion .
.
In summary this patient has severe organic disease which has well been documented including:
CERVICAL DISC HERNIATION
THORACIC SCOLIOSIS
THORACIC AV MALFORMATION
RIGHT SHOULDER IMPINGEMENT SYNDROME
PAIN SYNDROME DUE TO #1-4
Because of the medical conditions above, the inadvisability of surgery, and that medications used for the treatment and control of symptoms result in side effects including drowsiness, a complete to partial disability rating is warranted.